Understanding Rheumatoid Arthritis and How Synovial MSC Therapy May Treat It
- Mahdi Faour

- Jun 6, 2020
- 5 min read
Author: Suleiman Obeidat, Yr 12
The National Institutes of Health (NIH) estimated that in 2017, up to 23.5 million Americans suffered from autoimmune diseases, with evidence of increasing prevalence. Autoimmune diseases are a group of 80 or so chronic conditions that cause autoimmunity, where your immune system fails to differentiate between your normal healthy cells and harmful foreign cells which leads to the production of autoantibodies which target harmless self-antigens normally found in a healthy body. Rheumatoid arthritis (RA) is a type of autoimmune disease which causes inflammation in the tissues between joints. The immune system mistakenly attacks the tissue that lines the joints, which can cause pain, inflammation, swelling, and stiffness. This causes long term damage and loss of cartilage which can then over time damage the joint and the bone nearby. The condition can cause unbearable pain in the joints that can make it very difficult to move and complications can occur in many other parts of the body including blood vessels, skin, lungs, and skeletal muscle. There is no cure for RA but one therapy has shown a lot of potential in being able to treat the condition. Synovial MSC therapy uses a specific type of stem cells called mesenchymal stem cells (MSC) which have the potential of differentiating into cartilage and bone and so can be used to help treat inflamed and damaged joints.
Before understanding how synovial MSC therapy may be used to treat RA, it is worth (and quite interesting) first understanding the pathophysiology of the condition. Starting with the name, Arth- refers to joints and -itis refers to inflammation. Rheumatoid comes from rheumatism which is a broader term for musculoskeletal illness of the joints, bones, and cartilage. Normally, a health joint consists of bones covered with articular cartilage at the ends. Articular cartilage is a connective tissue that helps cushion and protect the ends of the bones by providing a lubricating surface so that bones can smoothly glide against each other during flexion or hyperextension of a joint. Synovial joints, like the knee joint or knuckle joint, also contain a fibrous joint capsule which connects the two bones and is continuous along the periosteum, or outer layer, of the bones. The capsule is lined with the synovial membrane, or synovium, which contains cells that produce synovial fluid, which is a viscous fluid that fills up the cavity of the joint and helps further lubricate it. Blood and lymph vessels in the synovial membrane help ensure that synovial cells are receiving the needed oxygen and nutrients to function properly.

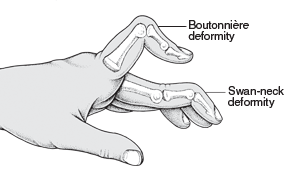
RA disrupts all that normal physiology. The actual cause of RA remains unknown, but it usually triggered by a combination of genetic and environmental factors. For example, individuals with certain genes such as HLA-DR1 and HLA-DR4 in the human leukocyte antigen (HLA) complex on chromosome 6 might be more susceptible to developing RA if exposed to environmental factors such as cigarette smoke or some specific pathogen. The HLA complex pretty much codes for antigens on white blood cells. The environmental factors can cause modification of proteins in our bodies such as immunoglobulin G (IgG), a type of antibody and type II collagen, which is what cartilage mainly consists of. Type II collagen is modified through a process called citrullination which is where the amino acid arginine is converted into citrulline. This is dangerous because the predisposed genes HLA-DR1 and HLA-DR4 causes our immune cells to not recognize the type II collagen and other structural proteins as self-antigens normally found in a healthy body. This causes the antigens to be carried by antigen presenting cells (APCs) to the lymph nodes which activates CD4+ T-Helper cells which in turn activates B-cells. The B-cells then rapidly multiply and differentiate into plasma cells which produces antibodies specific to the self-antigen, which in this case, include the type II collagen found in health joints. This triggers a series of cytokines being released from T-cells and macrophages (or phagocytes) which stimulate the synovial membrane to thicken and swell into what is called a pannus. This pannus can damage cartilage and erode bone which leads to weaker bones directly rubbing against each other causing chronic pain. Specific antibodies produced by plasma cells include Rheumatoid factor which binds to the Fc domain, or ‘body’ of IgG antibodies and Anti-CCP which binds to citrullinated proteins such as type II collagen. This leads to a series of immune responses which in turn cause chronic inflammation and damage to joints. Commonly affected joints are smaller joints like the metacarpo-phalangeal joints (MCPs) which are your knuckle joints and the proximal interphalangeal joints (PIPs) which are the first joints of your fingers. As the disease progresses, larger joints like the knees, shoulders, and elbows are also affected. There are many ways doctors may identify and diagnose RA. Patients with the condition may present specific deformities in the hands such as ulnar deviation, boutonniere deformity or swan neck deformity. Blood tests may be used to look for the presence of rheumatoid factor and anti-CCP antibodies. Additionally, x-rays may help reveal any decreased bone density, soft tissue swelling or narrowing of the painful joints.
So, how can stem cell therapy treat RA? As we have all learnt in school, stem cells are undifferentiated cell that can differentiate into different types of cells and maintain the ability to divide indefinitely. Mesenchymal stem cells (MSCs) are specific multipotent stem cells that can differentiate into a range of cells including osteocytes (bone cells) and chondrocytes (cartilage cells). MSCs can be mainly found in and extracted from the bone marrow but may also be found in other tissues such as fallopian tubes, peripheral blood, and fetal liver. Synovial MSC therapy consists of injecting these cells directly into the tissues surrounding the affected joints. The MSCs can then differentiate into cartilage and bone cells which would replace the damaged cells. In practice, a 2013 study (Wang et al. 2013) found encouraging results with RA patients who received MSC therapy experiencing “significant remission of disease”. However, this was a small sample and the therapy was not able to actually cure the disease. Dr Shane Shapiro, an orthopedic consultant in Mayo Clinic in the United States, notes that most research into MSC therapy has found that the treatment can help reduce symptoms and relief pain but very few studies have shown significant regrowth of bone or cartilage in order to fully treat RA. Synovial MSC therapy Is still in its very early stages and it may take years before a standard therapy is readily available to RA patients due to the difficulty of collecting MSCs and the strict guidelines around stem cell research which raises may raise some risks such as infection and immune rejection and some ethical issues if collected from embryos or fetal livers. However, the potential for stem cell therapy in treating autoimmune disease such as RA is substantial so optimism in the progression of science and technology…can go a long way.






Comments